Why is it better to have a lower heart rate?
Imagine doing a bicep curl a minimum of 40 but as many as 200 times every minute for your entire life (which is actually an interesting thought experiment). That’s exactly what our heart does — a muscle that contracts ~40 to ~200 times per minute from birth until death
The analogy isn’t perfect since skeletal and cardiac muscle are built differently, but it’s still pretty amazing. The slightest slip up in this system for even a couple minutes and you’re in the morgue, so not much room for error.
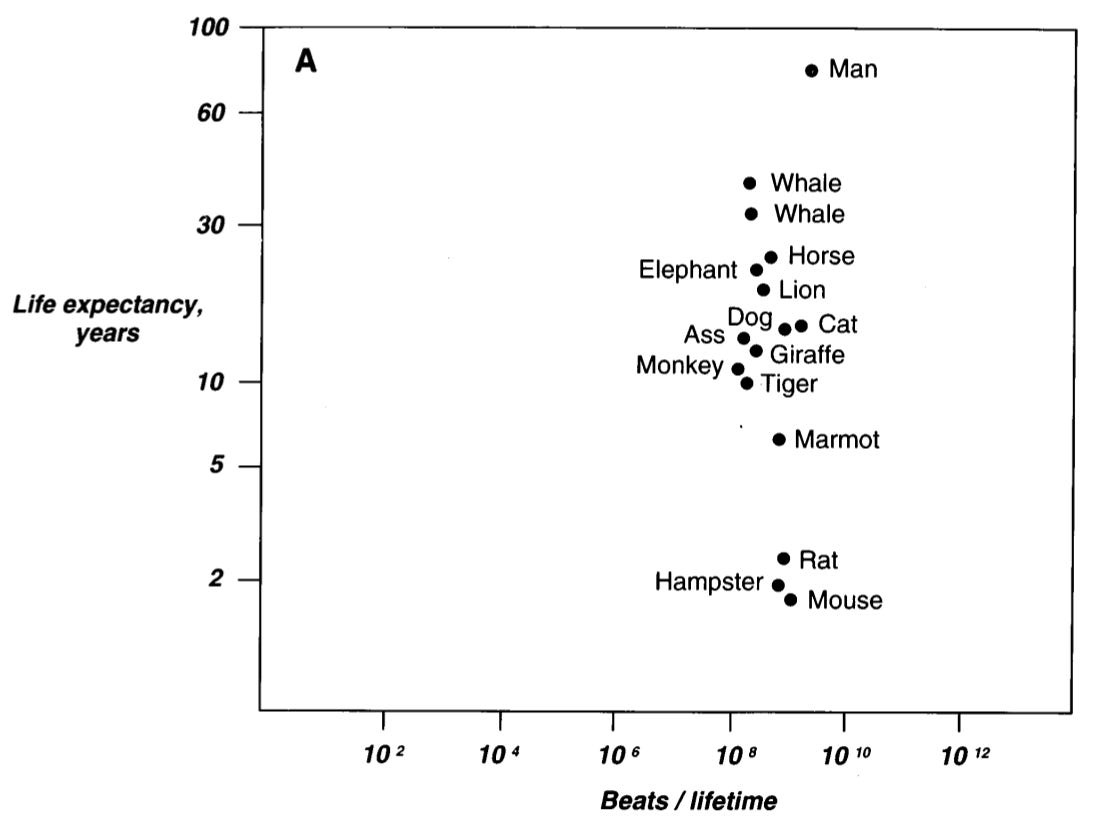
An interesting thought that has permeated for many years is that we (mammals) all get a certain number of heartbeats in our lifetime. About 1 billion, as you can see in the figure below (10^9). There are some confounding factors with this concept for sure, but what’s more relevant is that many studies show an increase in resting heart rate is associated with increased risk of death (references 2 & 3). Imagine the heart as a food runner
Each heartbeat sends blood to the body which carries oxygen and nutrients for our organs, whether we are sleeping or running an all-out mile. I used to work in restaurants so let’s compare the heart to a food runner. An all-out mile is the dinner rush with food flying out of the kitchen fast. As the night winds down and only a few tables are left, plates are sent out less frequently because demand is lower.
Being unfit is like a newly hired food runner who can only carry 1 plate at a time. They have to make several trips in and out of the kitchen each shift. But after a while, he gets more efficient and can carry 2-3 plates at a time. He moves a little slower but gets similar, if not more, work done, assuming we define productivity as the number of plates delivered each shift.
Plates delivered per shift = trips out of the kitchen * plates carried per tripIf he was a go-getter, he might eventually be able to move at the same fast rate, or faster, as when he was carrying 1 plate but is now carrying 2-3. Now productivity really booms.
The amount of plates delivered each shift is like the amount of blood we pump every minute, cardiac output. Cardiac output is a product of 2 things: 1) heart rate and 2) stroke volume (blood pumped per heart beat).
Cardiac output = heart rate * stroke volumeFor health and performance, a good cardiac output is really what we’re after. More blood, more oxygen, more speed.
How does cardiac output increase with training?
Wouldn’t it make sense that we should try to increase both our heart rate (trips out of the kitchen) and our stroke volume (plates per trip) to maximize cardiac output?
Well, if anything, our heart rate decreases as we get more fit, both at rest AND during exercise. An untrained person may have a maximal heart rate of 200 (this varies a tad between people) and a stroke volume of 100 (also varies a little, but I’m making the math easy), creating a maximal cardiac output of 20 liters per minute.
200 (heartbeats per minute) * 100 (milliliters per heartbeat) = 20,000 (milliliters of blood per minute), or 20 liters, of cardiac outputAnyone using a heart rate monitor will notice their heart rate does not go much above 180-200 even during your hardest efforts, no matter your fitness. That seems a bit odd, right? Why can’t it be 400 like a mouse or a rat?
If that math equation above is correct, increasing max heart rate by 20 beats would give you 2 extra liters of blood per minute. By 50 beats, 5 extra liters. And so on.
That seems like a pretty straightforward training adaptation and a way to increase cardiac output. But, it would only be true if stroke volume stayed the same (100 mL in the example).
Stroke volume and exercise training
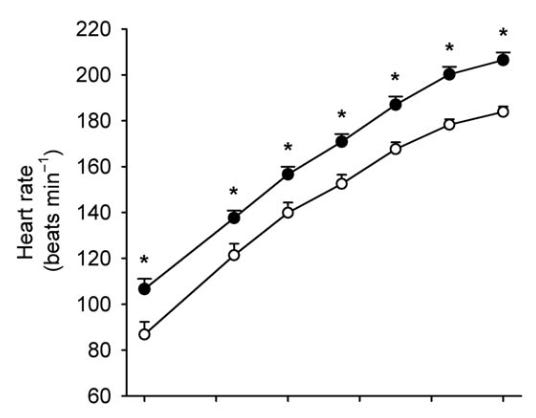
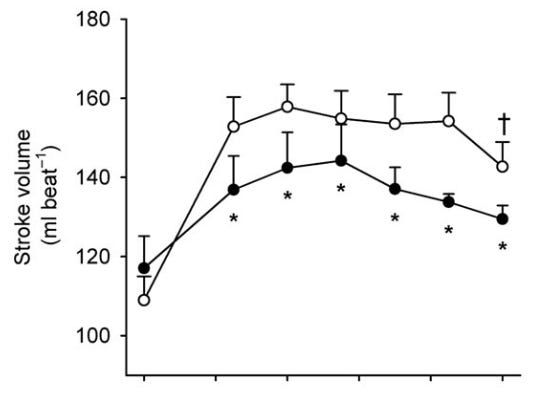
While a large cardiac output is a primary characteristic of elite athletes, the real player is stroke volume. Stroke volume is what allows attainment of such high cardiac output.
It’s not only that stroke volume is higher with improved fitness, but it also keeps increasing up to maximal exercise. In most people, stroke volume increases a little as we go out on a run, but there comes a point where it plateau’s. Years of training removes this plateau and allows stroke volume to increase along with intensity of exercise.
There are two main reasons for this. One is that the heart is very pliable and expands with training. When the pump is bigger you just can simply send out more blood. The other is speed at which the heart empties and fills with blood. The trained heart fills up, and empties, blood quicker with each heart beat.
Is maximal heart rate capped?
Scientists in my field are often interested in limiting factors in endurance performance because when you know what they are, you can devise ways to make them better and thus no longer be as limiting.
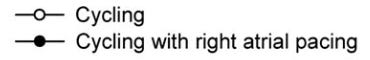
One group of researchers asked the question: “If I can make your heart beat faster, would cardiac output and performance be improved?”
The way they tested this using a technique called atrial pacing which involves snaking some catheters up to the heart and electrically stimulating it to beat at a specific rate. When the subjects were given ~20 extra heart beats at maximal exercise (184 versus 206), cardiac output didn’t change at all (25 liters per minute in both cases).
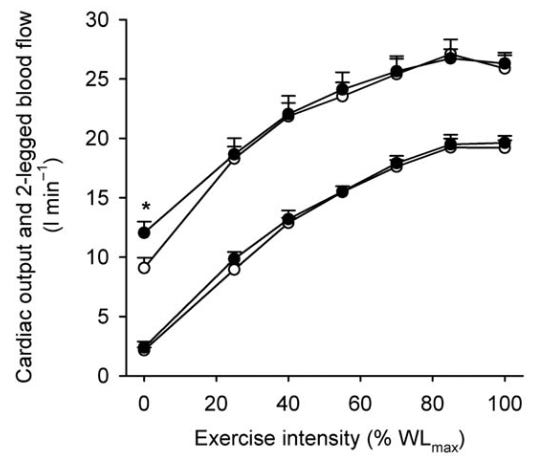
The only explanation then is that stroke volume decreased. They measured that too, and it did. We can take away from this that increasing maximal heart rate is counterproductive, unless stroke volume could stay the same.
Heart rates seem “capped” around 200 in humans* because the heart beat itself is “expensive”, metabolically speaking.
*Animals like mice and rats can have heart rates of 300-400.Why are heart beats “metabolically expensive”?
By metabolism I am referring to oxygen consumption (VO2). Something that is metabolically expensive costs more oxygen. Walking is cheaper than running. Running 10:00/mile is cheaper than 7:00/mile, and so forth.
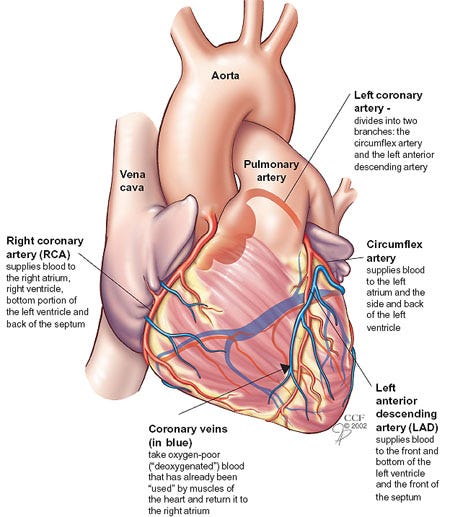
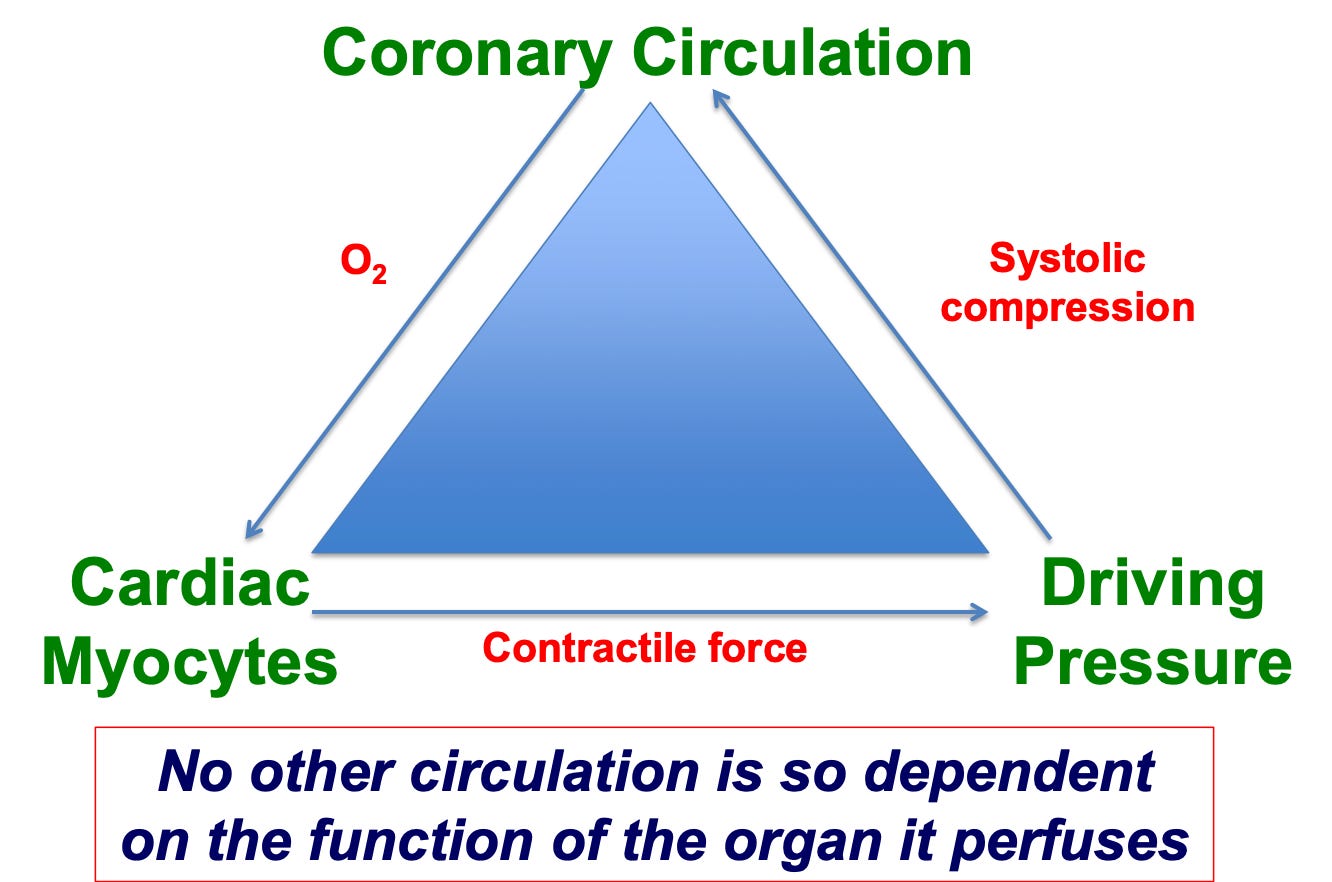
Remember that the heart must pump blood to all organs so they can consume oxygen for their functions. That includes the heart itself, and it does so using the coronary arteries. These are the ones that get clogged from bad lifestyle habits and lead to heart attacks. There are about 3-4 things that influence the heart’s VO2, and heart rate has the biggest influence. Whatever the heart’s oxygen consumption is, heart rate is responsible for 50-70% of it.
To fully understand this question we need to delve into blood pressure briefly.
Blood pressure has 2 phases, systole (sis-toe-lee; high pressure) and diastole (die-ass-toe-lee; low pressure). Right after the heart contracts (beats) and blood rushes through the arteries, we’re in systole, then it relaxes and we’re in diastole.
Tissues like the heart and skeletal muscle take up most of their blood during diastole (the proper term is tissue perfusion), because during the high-pressure systolic phase, small blood vessels (capillaries) that exchange oxygen and nutrients, get compressed.
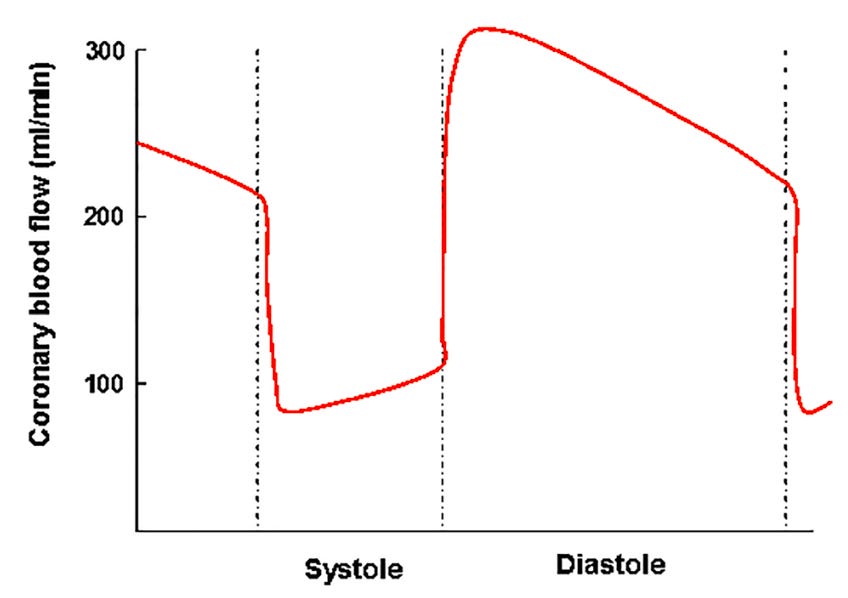
As heart rate increases we spend more time in systole. More time in systole means less in diastole and thus less blood flow. We need blood flow to support oxygen consumption or VO2. This creates a tricky scenario where our heart beats faster because we’re intensely exercising, which increases the heart’s VO2, but those faster heart beats also threaten the heart’s own blood supply.
A mismatch between our heart’s oxygen demand (VO2) and supply (blood flow) results in ischemia (lack of oxygen), which can quite literally kill pieces of our heart muscle.
Nature likely designed each person’s maximal heart rate to be set as high as possible without threatening coronary blood flow. It’s like a built-in protection mechanism, and recently a scientist from Finland put forward a hypothesis for how it works and the limiting factors for cardiac output.
When you decrease the heart rate you decrease the metabolic stress on the heart, so it now requires less oxygen, spends more time in diastole, and decreases the chances of interrupted blood flow. Athlete heart’s are also much larger and the VO2 per gram of heart tissue is lower in athletes. This creates a greater functional reserve, or greater potential to increase blood flow when needed.
Myocardial blood flow and exercise training
Unlike skeletal muscle, endurance athletes have lower myocardial (heart muscle) blood flow. However, blood within the heart hangs around for a longer time. The “hanging around” is called the mean transit time, and when blood has a longer transit time there is more time for oxygen and nutrients to be exchanged.
Think of the mean transit time like riding the subway. There are 100 total people at station A and 100 people at station B waiting to get on. Train A stops and opens its doors for 10 seconds, while train B stops for 15 seconds.
70 people make it on train A, while 80 people make it on train B because they had a little more time. Train B “extracts” more people from the station. Train B is the athlete’s heart.
In this example, the train is the blood, the tunnel is the blood vessel, and the people are oxygen molecules. The trained heart indeed can pull more oxygen out of the blood passing through the arteries and capillaries, which is called oxygen extraction. In one study, athletes could grab about 10% more oxygen out of blood vessels than regular people.
Take home message
If you’re like me and are curious about “why” things happen in our body, I hope you enjoyed this. A decrease in resting and exercising heart rate is a good thing. It’s necessary for improved performance. It relieves our heart from high metabolic demand which could make it ischemic, and allows very large stroke volumes to be obtained, which in turn improve aerobic capacity. And, less heartbeats seem tied to a longer life.
References
Rest heart rate and life expectancy. Journal of the American College of Cardiology, 30(4), 1104–1106.
Change in resting heart rate and risk for all-cause mortality. European journal of preventive cardiology, 29(7), e249–e254.
Resting heart rate, cardiovascular events, and all-cause mortality: the REGICOR study. European journal of preventive cardiology, 29(5), e200–e202.
Maximal heart rate does not limit cardiovascular capacity in healthy humans: insight from right atrial pacing during maximal exercise. The Journal of physiology, 592(2), 377–390.
Myocardial blood flow and its transit time, oxygen utilization, and efficiency of highly endurance-trained human heart. Basic research in cardiology, 109(4), 413.
Endurance athletes' stroke volume does not plateau: major advantage is diastolic function. Medicine and science in sports and exercise, 26(9), 1116–1121.
Cardiac output limits maximal oxygen consumption, but what limits maximal cardiac output?. Experimental physiology, 10.1113/EP091594.
Regulation of coronary blood flow during exercise. Physiological reviews, 88(3), 1009–1086.
Sean Langan has his PhD in exercise physiology and currently works as a research physiologist. He is interested in endurance and strength training, and harnessing the intersection of human physiology, technology, research, and coaching to improve human performance. Sean writes about various topics specific to his personal interests and observations, but if there is anything specific you would like to see please contact him.